Sleep–Wake Disorders Including Insomnia
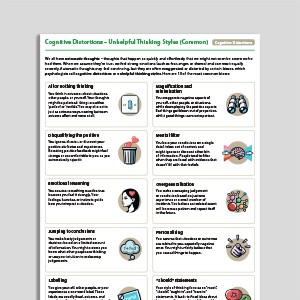
Cognitive Distortions – Unhelpful Thinking Styles (Common)
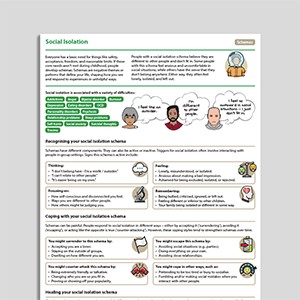
Social Isolation
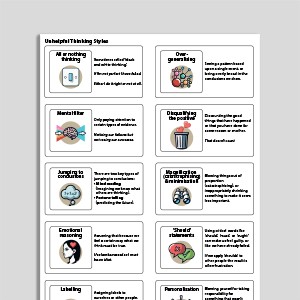
Unhelpful Thinking Styles (Archived)
Audio Collection: Psychology Tools For Relaxation
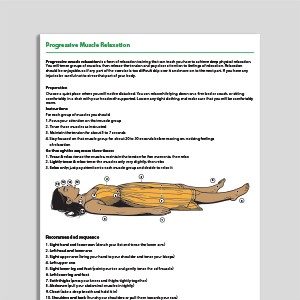
Progressive Muscle Relaxation
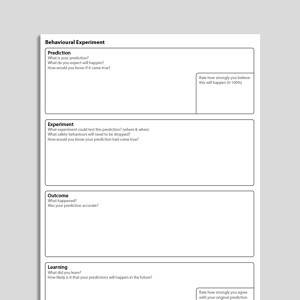
Behavioral Experiment (Portrait Format)
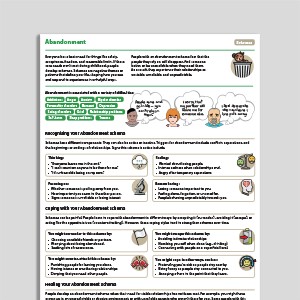
Abandonment
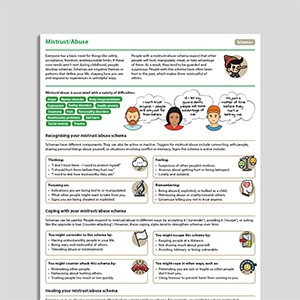
Mistrust/Abuse
Guidelines For Better Sleep
Behavioral Experiment
Pessimism
Nightmare Exposure And Rescripting
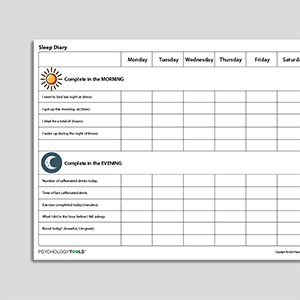
Sleep Diary
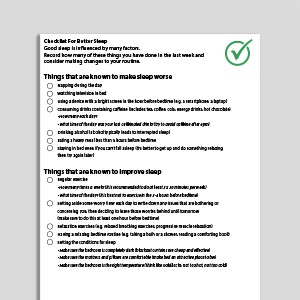
Checklist For Better Sleep
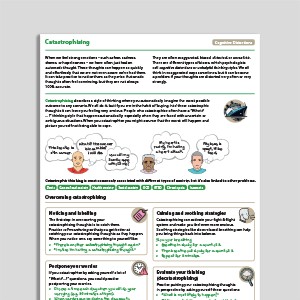
Catastrophizing
Progressive Muscle Relaxation (Audio)
Learning To Relax (CYP)
Entitlement
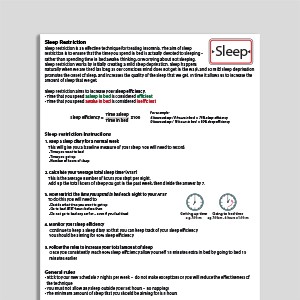
Sleep Restriction
Relaxed Breathing Exercise 1 (Audio)
Progressive Muscle Relaxation (Archived)
Combined Relaxation Exercise (Audio)
Peaceful Place (Audio)
Overcoming Insomnia (Second Edition): Workbook
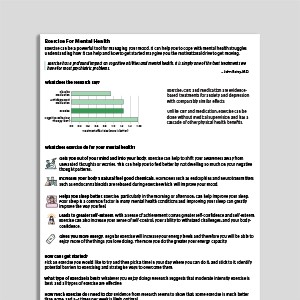
Exercise For Mental Health
Overcoming Insomnia (Second Edition): Therapist Guide
Nightmare Rescripting (Audio)
Sleep Hygiene (Audio)
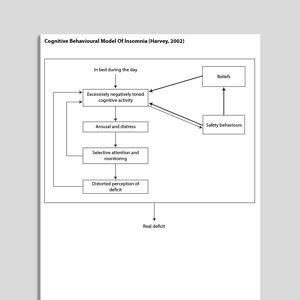
Cognitive Behavioral Model Of Insomnia (Harvey, 2002)
Relaxed Breathing Exercise 4 (Audio)
Relaxed Breathing Exercise 2 (Audio)
Relaxed Breathing Exercise 3 (Audio)
Recovering From A Nightmare (Audio)
Recognizing Insomnia Disorders
Links to external resources
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
Assessment
-
Epworth Sleepiness Scale (ESS)
| Johns | 1991
- Scale
- Johns, M. W. (1991). A new method for measuring daytime sleepiness: the Epworth sleepiness scale. sleep, 14(6), 540-545.
-
Pittsburgh Sleep Quality Index (PSQI)
| Buysse, Reynolds, Monk, Berman, Kupfer | 1989
- Scale
- Buysse, D. J., Reynolds III, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research, 28(2), 193-213.
Guides and workbooks
- Improve your sleep: a self-guided approach for veterans with insomnia | MIRECC
Information Handouts
-
Sleep (Information Handouts)
| Centre For Clinical Information
- Facts About Sleep
- What Is Insomnia?
- Insomnia and Your Thinking
- Sleep Hygiene
- Nightmares Explained
- What Is Imagery Rescripting?
- Sleep stimulus control – essential component of CBT treatment for sleep problems | GoodMedicine
- Sleep restriction instructions | APA
- Sleeping advice – generic sleep hygeine advice | GoodMedicine
Presentations
- Sleeping your way to better mental health | Sophie Bostock | 2015
- Cognitive behavioral therapy for insomnia | Melanie Leggett | 2014
- Insomnia | Victoria Judd
- CBT for insomnia | Virginia Runko
- Cognitive behavioural therapy for insomnia: what it is & what it does | Colin Espie
Treatment Guide
-
Overcoming insomnia: a 5 session, interactive CBT program for overcoming insomnia
| 2005
- Session 1: Basic facts about sleep, understanding your own insomnia
- Session 2: Sleep scheduling and stimulus control techniques
- Session 3: Changing your thoughts and learning how to stop using sleeping pills
- Session 4: Daytime relaxation techniques and stress-reducing attitudes and beliefs
- Session 5: Bedtime relaxation techniques, lifestyle practices for improving sleep
- Cognitive behavioral therapy for insomnia (CBTi) treatment manual | Munoz, Miranda, McQuaid, Sze, Otilingham
- Cognitive-Behavioral Insomnia Therapy | Jack Edinger
- Getting better sleep workbook | Good Thinking
Worksheets
- Sleep Diary | Centre For Clinical Interventions
Recommended Reading
- Imagery rehearsal therapy: principles and practice | Krakow, B., & Zadra, A. | 2010
- van Straten, A., & Cuijpers, P. (2009). Self-help therapy for insomnia: a meta-analysis. Sleep Medicine Reviews, 13(1), 61-71
- Sheaves, B., Isham, L., Bradley, J., Espie, C., Barrera, A., Waite, F., … & Freeman, D. (2018). Adapted CBT to stabilize sleep on psychiatric wards: a transdiagnostic treatment approach.Behavioural and cognitive psychotherapy,46(6), 661-675.
- Okajima, I., Komada, Y., & Inoue, Y. (2011). A meta‐analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep and Biological Rhythms, 9(1), 24-34
- Kyle, S. D., Aquino, M. R. J., Miller, C. B., Henry, A. L., Crawford, M. R., Espie, C. A., & Spielman, A. J. (2015). Towards standardisation and improved understanding of sleep restriction therapy for insomnia disorder: a systematic examination of CBT-I trial content.Sleep medicine reviews,23, 83-88.
- Edinger, J. D., & Means, M. K. (2005). Cognitive–behavioral therapy for primary insomnia. Clinical Psychology Review, 25(5), 539-558
What Are Sleep Problems?
Symptoms Associated with Poor Sleep and Insomnia
Insomnia disorder is characterized by a complaint of dissatisfaction with sleep quantity or quality, associated with one or more of:
- difficult initiating sleep
- difficulty maintaining sleep
- early-morning awakening with inability to return to sleep
Nightmare disorder is characterized by repeated occurrences of extended, extremely dysphoric, and well-remembered dreams which usually involve efforts to avoid threats to survival, security, or physical integrity. The individual rapidly becomes oriented and alert upon awakening. The dreams are not better explained by the presence of other conditions such as post-traumatic stress disorder.
Psychological Models and Theory of Insomnia
A range of psychological models of insomnia are reviewed in detail in Talbot and Harvey (2010).
Spielman’s Three-P Model of Insomnia (Spielman, Saskin, & Thorpy, 1987)
Spielman’s three-factor model is a diathesis-stress theory that includes predisposing, precipitating, and perpetuating factors influencing insomnia. Perpetuating factors are the typical targets for treatment and include: maladaptive coping skills, and an extension of time in bed. Spielman’s three-P model led to the development of the sleep restriction technique for insomnia.
Bootzin’s Stimulus Control Model of Insomnia (1972)
The stimulus control model of insomnia proposes that the particular response elicited by a stimulus depends upon its conditioning history. Insomnia is said to occur when sleep stimuli (e.g., bed, bedroom, bedtime) are no longer uniquely paired with sleep, but have been paired with other activities (e.g., worrying, being awake, reading). Stimulus control therapy is an effective intervention derived from stimulus control theory.
Espie’s Psychobiological Inhibition Model of Insomnia (2002; Espie, Broomfield, MacMahon, Macphee, & Taylor, 2006)
Espie’s psychobiological inhibition model of insomnia proposes that homeostatic and circadian processes are involuntary and the normal default result is good sleep. Good sleep is maintained by regular sleep habits, sleep-related physiological de-arousal, and sleep-related cognitive de-arousal. According to this model, insomnia is the result of interruptions to or failures of these maintenance processes. An updated version of the model proposes that people can interfere with automatic processes resulting in good sleep by: selectively attending to sleep, explicitly intending to sleep, trying to sleep. Interventions derived from the model target these dysfunctional processes (Espie et al., 2006).
Harvey’s Cognitive Model of Insomnia (2002)
Harvey proposes that insomnia is maintained by a cascade of five critical cognitive processes including: worry (accompanied by arousal and distress); selective attention and monitoring; misperception of sleep and daytime deficits from lack of sleep; unhelpful beliefs; and counterproductive safety behaviors. Treatment interventions for insomnia targets these maintaining mechanisms.
Evidence-Based Psychological Approaches for Working with Insomnia
Evidence-based psychological approaches for working with insomnia include:
- sleep restriction therapy
- stimulus control therapy
- cognitive behavioral therapy for insomnia (CBT-I)
Resources for Working with Sleep–Wake Disorders Including Insomnia
Psychology Tools resources available for working therapeutically with sleep–wake disorders including insomnia include:
- psychological models of sleep–wake disorders including insomnia
- information handouts for sleep–wake disorders including insomnia
- exercises for sleep–wake disorders including insomnia
- CBT worksheets for sleep–wake disorders including insomnia
- self-help programs for sleep–wake disorders including insomnia
References
- Bootzin, R. R. (1972). Stimulus control treatment for insomnia. Proceedings of the American Psychological Association, 7, 395–396.
- Espie, C. A. (2002). Insomnia: Conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annual Review of Psychology, 53, 215–243.
- Espie, C. A., Broomfield, N. M., MacMahon, K. M., Macphee, L. M., & Taylor, L. M. (2006). The attention-intention-effort pathway in the development of psychophysiologic insomnia: A theoretical review. Sleep Medicine Review, 10(4), 215–245.
- Harvey, A. G. (2002). A cognitive model of insomnia. BehaviourResearch and Therapy, 40(8), 869–894.
- Sheaves, B., Freeman, D., Isham, L., McInerney, J., Nickless, A., Yu, L. M., … & Barrera, A. (2018). Stabilisingsleep for patients admitted at acute crisis to a psychiatric hospital (OWLS): An assessor-blind pilot randomisedcontrolled trial. Psychological Medicine,48(10), 1694–1704.
- Spielman, A. J., Saskin, P., & Thorpy, M. J. (1987). Treatment of chronic insomnia by restriction of time in bed.Sleep, 10(1), 45–56.
- Talbot, L. S., & Harvey, A. G. (2010). Psychological models of insomnia. In M. J. Sateia and D. Buysse (Eds.), Insomnia: Diagnosis and Treatment(pp. 42–49). Boca Raton, FL: CRC Press.