Obsessive Compulsive Disorder (OCD) including Body Dysmorphic Disorder (BDD)

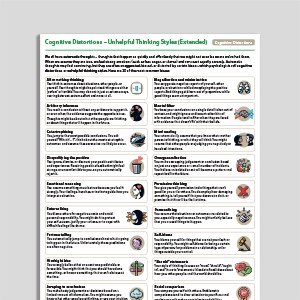
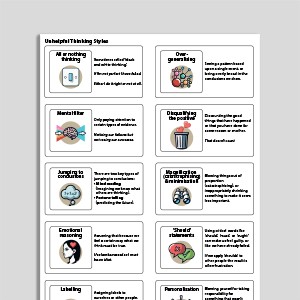
Cognitive Distortions – Unhelpful Thinking Styles (Extended)
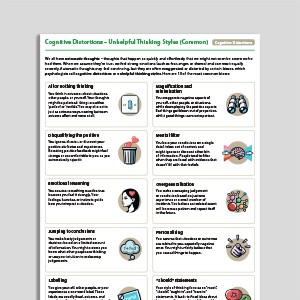
Cognitive Distortions – Unhelpful Thinking Styles (Common)
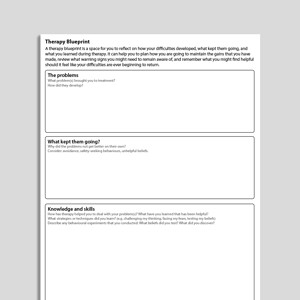
Therapy Blueprint (Universal)
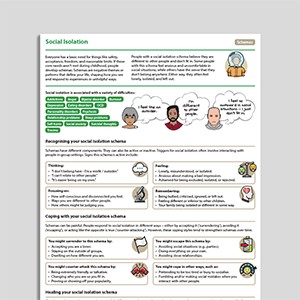
Social Isolation
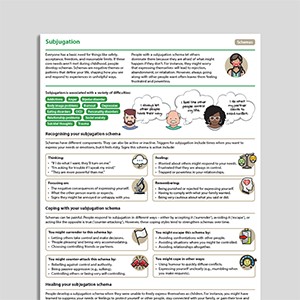
Subjugation
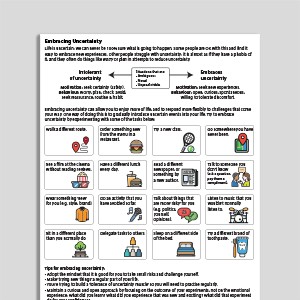
Embracing Uncertainty
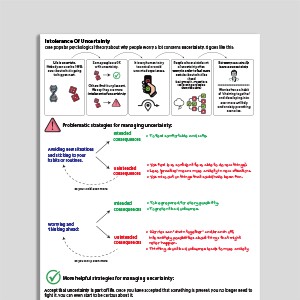
Intolerance Of Uncertainty
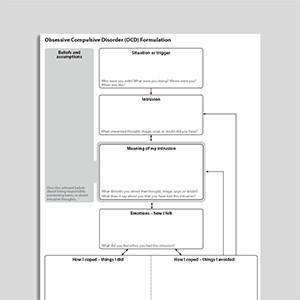
Obsessive Compulsive Disorder (OCD) Formulation
Unhelpful Thinking Styles (Archived)
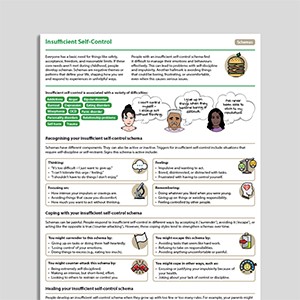
Insufficient Self-Control
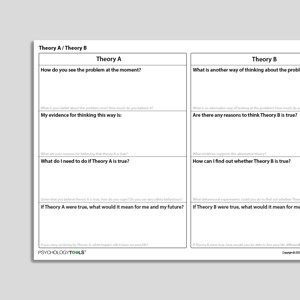
Theory A / Theory B
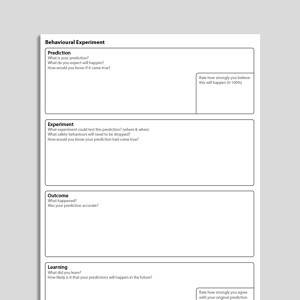
Behavioral Experiment (Portrait Format)
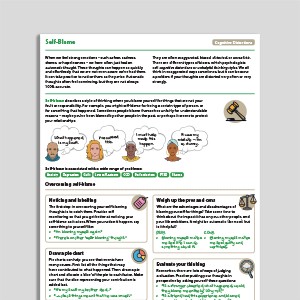
Self-Blame
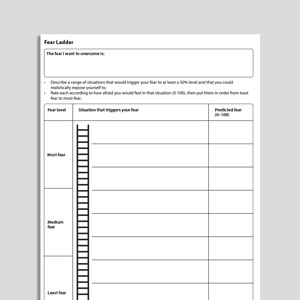
Fear Ladder
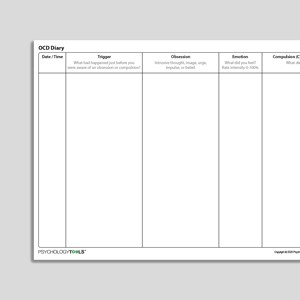
OCD Diary
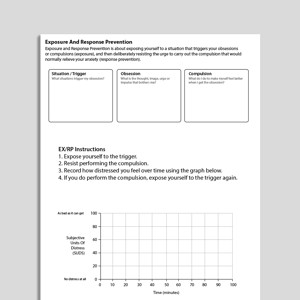
Exposure And Response Prevention
Behavioral Experiment
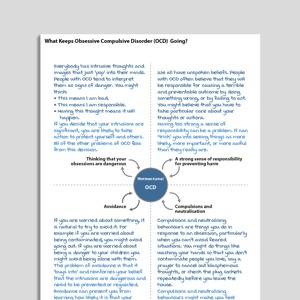
What Keeps Obsessive Compulsive Disorder (OCD) Going?
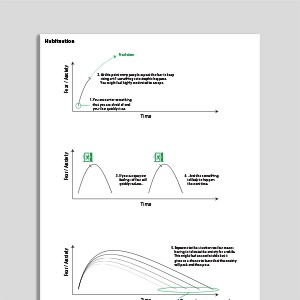
Habituation
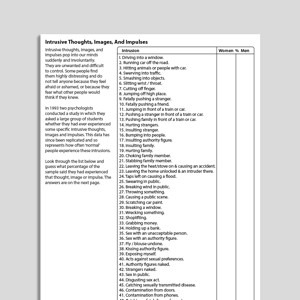
Intrusive Thoughts Images And Impulses
Understanding Obsessive Compulsive Disorder (OCD)
Treating Your OCD With Exposure And Response (Ritual) Prevention (Second Edition): Workbook
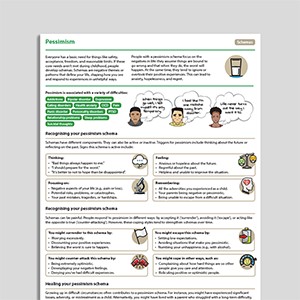
Pessimism
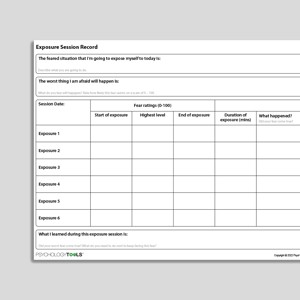
Exposure Session Record
Punitiveness
Failure To Achieve
OCD Hierarchy
Catastrophizing
"Should" Statements
Thought-Action Fusion
Emotional Reasoning
Thought Suppression And Intrusive Thoughts
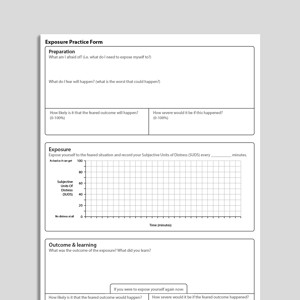
Exposure Practice Form
Emotional Inhibition
Approval-/Admiration-Seeking
Self-Monitoring Record (Universal)
Defectiveness
Exposure And Response (Ritual) Prevention For Obsessive Compulsive Disorder (Second Edition): Therapist Guide
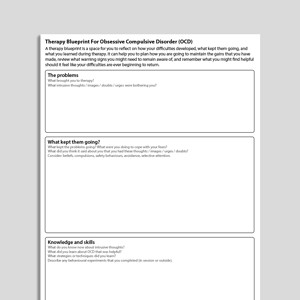
Therapy Blueprint For OCD
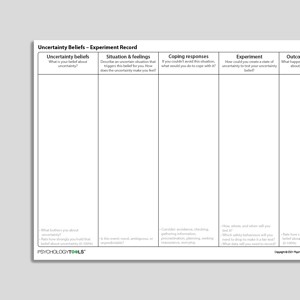
Uncertainty Beliefs – Experiment Record
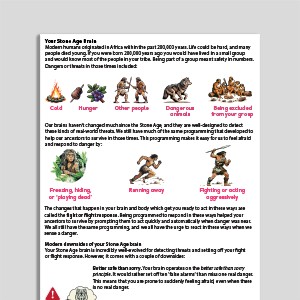
Your Stone Age Brain
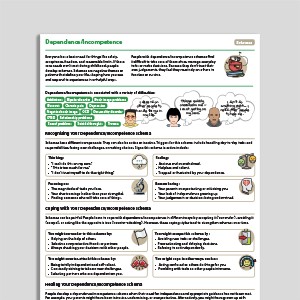
Dependence / Incompetence
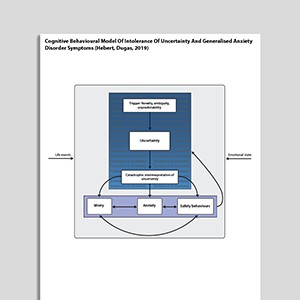
Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)
Intrusive Memory Record
Checking Certainty And Doubt
Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm: Workbook
Recognizing Obsessive Compulsive Disorder (OCD)
Disqualifying The Positive
Cognitive Behavioral Treatment Of Childhood OCD: It's Only A False Alarm: Therapist Guide
What Is Exposure Therapy?
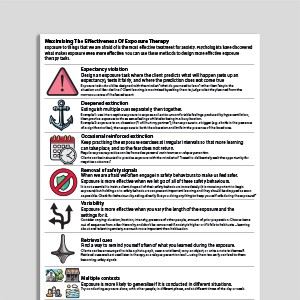
Maximizing The Effectiveness Of Exposure Therapy
Facing Your Fears And Phobias
Intrusion Record
Avoidance Hierarchy (Archived)
Urges – Self-Monitoring Record
Understanding Body Dysmorphic Disorder
Am I Experiencing Obsessive Compulsive Disorder (OCD)?
What Keeps Body Dysmorphic Disorder (BDD) Going?
Personalizing
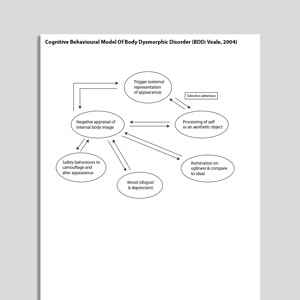
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)
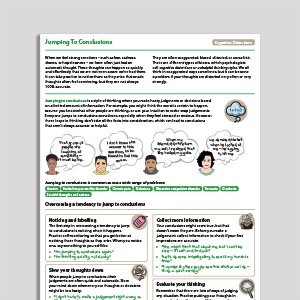
Jumping To Conclusions
What Is Body Dysmorphic Disorder (BDD)?
Links to external resources
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
Assessment
-
Obsessive Beliefs Questionnaire (OBQ-44)
| Obsessive Compulsive Cognition Working Group | 2001
- Scale
- Obsessive Compulsive Cognition Working Group. (2001). Development and initial validation of the Obsessive Beliefs Questionnaire and the Interpretation of Intrusions Inventory. Behaviour Research and Therapy, 39, 987–1006.
OCD
- Obsessive Compulsive Inventory (OCI) scoring grid
- Relationship Obsessive Compulsive Inventory (ROCI)
- Partner Related Obsessive Compulsive Symptom Inventory
- OCD Trauma Timeline Interview (OTTI) | Wadsworth, Van Kirk,August, MacLaren Kelly, Jackson, Nelson & Luehrs | 2023
- Vancouver Obsessional Compulsive Inventory (VOCI)
Guides and workbooks
- What you need to know about OCD | International OCD Foundation (IOCDF)
- Managing obsessive compulsive disorder | Simon Enright
- Obsessive compulsive disorder: patient treatment manual | Clinical Research Unit for Anxiety and Depression (CRUfAD)
- OCD: An OCD-UK Information Guides For People Affected By Obsessive Compulsive Disorder | OCD-UK
- Self-Help: Managing Your OCD At Home | Anxiety Canada
Information Handouts
- "Just Right" OCD Symptoms | IOCDF | 2009
- What are postpartum and perinatal OCD? | IOCDF
Information (Professional)
- Scrupulosity and OCD: information packet for faith leaders | IOCDF, ADAA
Presentations
- Cognitive behavioral therapy for OCD | Sabine Wilhelm
- New directions in implementing exposure and response prevention: an inhibitory learning perspective | Jonathan Abramowitz | 2018
- Cognitive Therapy for Contamination-Related OCD: ERP and Beyond | Adam Radomsky | 2011
- Interoceptive exposure: an underused weapon in the arsenal against obsessions and compulsions | Jonathan Abramowitz | 2018
- Family affair: involving a partner or spouse in exposure and response prevention for OCD | Jonathan Abramowitz | 2018
- A couple-based approach to CBT for BDD | Lillian Reuman, Jonathan Abramowitz | 2016
- Body dysmorphic disorder | David Veale | 2017
Treatment Guide
- NICE Guidelines For OCD and BDD | NICE | 2005
- Treatment of patients with OCD | American Psychiatric Association (APA) | 2007
- Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders (2014) | Katzman et al | 2014
- A psychological perspective on hoarding – DCP good practice guidelines | Holmes, S., Whomsley, S., Kellet S. | 2015
- Treatment Manual For OCD | Clinical Research Unit for Anxiety Disorders (CRUFAD) | 2010
Recommended Reading
BDD
- Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image ,1, 113-125
OCD
- Gillihan, S., Williams, M. T., Malcoun, E., Yadin, E., Foa, E. B. (2012) Common pitfalls in exposure and response prevention (EX/RP) for OCD. Journal of Obsessive-Compulsive and Related Disorders, 1, 251-257
- Rachman, S. (1997). A cognitive theory of obsessions. Behaviour Research and Therapy, 35(9), 793-802
- Mataix-Cols, D., et al (2010). Hoarding disorder: A new diagnosis for DSM-V? Depression and Anxiety, 27, 556-572.
- Salkovskis, P. (1999). Psychological treatment of obsessive–compulsive disorder. Behaviour Research and Therapy, 37, S37-S52
- Salkovskis, P. M. (2007). Psychological treatment of obsessive–compulsive disorder.Psychiatry,6(6), 229-233
- Veale, D. (2007). Cognitive behavioural therapy for obsessive compulsive disorder. Advances in Psychiatric Treatment. 13, 438-446
- Veale, D., Freeston, M., Krebs, G., Heyman, I., & Salkovskis, P. (2009). Risk assessment and management in obsessive–compulsive disorder. Advances in psychiatric treatment, 15(5), 332-343.
BDD
- Danesh, M., Beroukhim, K., Nguyen, C., Levin, E., & Koo, J. (2015). Body dysmorphic disorder screening tools for the dermatologist: A systematic review.Pract Dermatol,2, 44-49.
- Krebs, G., de la Cruz, L. F., & Mataix-Cols, D. (2017). Recent advances in understanding and managing body dysmorphic disorder. Evidence-Based Mental Health, 20(3), 71-75.
OCD
- Doron, G., & Derby, D. (2015). Assessment and treatment of relationship-related OCD symptoms (ROCD): a modular approach. Handbook of Obsessive-Compulsive Disorder across the Lifespan. Hoboken, NJ: Wiley (Forthcoming).
BDD
- Veale, D. (2001). Cognitive-behavioural therapy for body dysmorphic disorder. Advances in Psychiatric Treatment, 7, 125-132
- Assessment and treatment of relationship-related OCD symptoms | Guy Doron, Danny Derby | 2017
OCD
- Clark, D. A., & Rhyno, S. (2005). Unwanted intrusive thoughts in nonclinical individuals. Intrusive thoughts in clinical disorders: Theory, research, and treatment, 1-29
What Is Obsessive Compulsive Disorder?
Signs and Symptoms of OCD
People with OCD experience obsessional thoughts, images, urges, and doubts. They often feel compelled to act or think in certain ways.
Obsessions are intrusive thoughts—thoughts that are unwanted and unacceptable, and which pop into our minds unbidden. Obsessions can be thoughts in the form of words, but also of images (pictures in our minds), urges or impulses, or feelings of doubt. Obsessive thoughts are experienced as unacceptable, disgusting, or senseless, and people with OCD find it hard not to pay attention to them. Examples of obsessions include:
- thoughts such as ‘My hands have been contaminated with germs’ or ‘Perhaps I am a pedophile’
- images of my family being murdered
- doubts such as ‘Have I left the stove on?’
- urges such as wanting to shout profanities
Compulsions follow from the way in which the individual interprets the intrusive thoughts. Compulsions are the reactions or mental actions that a person does in order to neutralize or ‘make safe’ following an obsession. People with OCD typically carry out compulsions in order to prevent a harm from happening for which they might be responsible, and/or to reduce any strong emotion which they feel. Exactly what someone with OCD may feel compelled to do will depend upon the meaning their intrusions have for them. Examples of compulsions might include:
- carefully washing food after having an intrusive thought about germs;
- calling family members to check they are OK after having an intrusive image about their deaths;
- going back to the house to check after doubting whether the stove was turned off;
- avoiding a public place after having an urge to shout profanities.
Prevalence of OCD
The lifetime prevalence rate of OCD in the United States is estimated to be 2.3% in adults (Kessler et al., 2005), and 1% to 2.3% in children and adolescents (Zohar, 1999).
Psychological Models and Theory of OCD
The cognitive behavioral theory of OCD proposes that when someone experiences an intrusive thought it is the appraisal—what they make of having the thought—that is most important (Salkovskis, Forrester, & Richards, 1998). Intrusive thoughts, even very unpleasant ones, are common and entirely normal. What seems to happen in OCD is that the fact of having intrusive thoughts is interpreted as being especially significant and, as a result, is especially anxiety-provoking. People with OCD are more likely to feel especially responsible for any potential harms and may feel especially strong emotion should they have intrusive thoughts about harm occurring. Compulsions are understood to be an active attempt to reduce harm. According to the cognitive model of OCD targets for intervention include:
- understanding and addressing the meaning of the intrusions;
- targeting compulsions and safety-seeking behaviors;
- modifying attentional biases.
Evidence-Based Psychological Approaches for Working with OCD
Cognitive behavioral therapy (CBT) is an evidence-based psychological treatment for OCD. Historically, CBT for OCD has involved the behavioral approach of exposure with response prevention (ERP). More cognitive approaches within CBT attempt to understand the patient’s appraisal of their intrusions and to find ways of exploring the validity and consequences of these appraisals.
Resources for Working with OCD
Psychology Tools resources available for working therapeutically with OCD may include:
- psychological models of obsessive-compulsive disorder (OCD)
- information handouts for obsessive-compulsive disorder (OCD)
- exercises for obsessive-compulsive disorder (OCD)
- CBT worksheets for obsessive-compulsive disorder (OCD)
- self-help programs for obsessive-compulsive disorder (OCD)
References
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602.
- Salkovskis, P. M., Forrester, E., & Richards, C. (1998). Cognitive–behavioral approach to understanding obsessional thinking. The British Journal of Psychiatry, 173(S35), 53–63.
- Zohar, A. H. (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 8(3), 445–460.