Cognitive Behavioral Therapy (CBT)
Cognitive behavior therapy (CBT) is a popular form of psychological therapy that works with our thoughts, feelings, and behaviors. CBT is an integration of principles from behavior therapy with theory and methods from the cognitive therapies developed by Aaron Beck and Albert Ellis. The CBT that is practiced today has evolved with new developments in basic and applied research; it is grounded in empirical research and clinical practice. CBT is a broad church: the family of ‘cognitive and behavioral therapies’ encompasses many approaches including cognitive therapy, acceptance and commitment therapy (ACT), dialectical behavior therapy (DBT), and compassion-focused therapy (CFT).
Beck’s cognitive model identifies different levels of human cognitions: automatic thoughts are the most superficial level of cognition and describe the thoughts, words, ideas, and images that seem to pop into our minds; rigid and over-generalized core beliefs about ourselves, the world, and other people; and intermediate attitudes, rules, and assumptions that are influenced by our core beliefs. The cognitive model proposes that how we feel emotionally, and how we act, are determined by how we interpret and think about a situation. It argues that psychological problems and disorders are the result of dysfunctional thinking, and are maintained by self-defeating behavior influenced by inaccurate beliefs. Cognitive behavior therapists understand that by changing the way we think and act in the here-and-now we can change the way we feel, and CBT often begins with a focus on what is maintaining a problem in the present. For lasting change, CBT therapists often work with the deeper levels of their client’s beliefs and assumptions. Read more
3 of 303 resources
What Is Bulimia?
Our ‘What Is … ?’ series is a collection of one-page information handouts for common mental health conditions. Friendly and explanatory, handout ...
https://www.psychologytools.com/resource/what-is-bulimia/
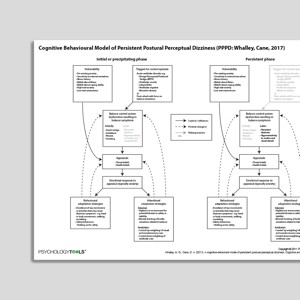
Cognitive Behavioral Model Of Persistent Postural-Perceptual Dizziness (PPPD: Whalley, Cane, 2017)
Persistent postural-perceptual dizziness (PPPD) is a form of dizziness which is thought to be maintained by psychological factors. This is a Cognitive ...
https://www.psychologytools.com/resource/cognitive-behavioral-model-of-persistent-postural-perceptual-dizziness-pppd-whalley-cane-2017/
Putting It All Together (Psychology Tools For Living Well)
Cognitive behavioral therapy can help your clients to live happier and more fulfilling lives. Psychology Tools for Living Well is a self-help course ...
https://www.psychologytools.com/resource/putting-it-all-together-psychology-tools-for-living-well/
Links to external resources
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
Assessment
-
Supervisor Competency Scale (SCS)
| Kennerley, Clohessy, Butler, Muse, Rakovshik | 2014
- Scale
- Bern Inventory of Treatment Goals | Grosse, Grawe | 2002
Cognitive therapy competence / adherence measures
-
Revised Cognitive Therapy Scale (CTS-R) – James, Blackburn, Reichelt Scale Manual
- Manual
- Scale
-
Cognitive Therapy Rating Scale (CTRS)
| Young, Beck | 1980
- Scale
- Manual
-
Assessment of Core CBT Skills (ACCS)
| Muse, McManus, Rakovshik, Kennerley
- Manual accs-scale.co.uk
- Feedback form accs-scale.co.uk
- Website accs-scale.co.uk
Case Conceptualization / Case Formulation
- Cognitive conceptualisation (excerpt from Basics and Beyond) | J. Beck
- Dysfunctional assumptions ideas
- Developing a cognitive formulation | Michael Free
- Case formulation in CBT | Caleb Lack
- A case formulation approach to cognitive-behavior therapy | Jacqueline Persons | 2015
- The case formulation approach to cognitive behavior therapy | Jacqueline Persons | 2014
Information (Professional)
- Cognitive- behavioural therapy An information guide | Neil Rector | 2010
- A therapist’s guide to brief cognitive behavioral therapy | Cully, Teten | 2008
- Problem solving (OCT Practical Guides | Helen Kennerley | 2016
- Working with Schemas, Core Beliefs, and Assumptions | Frank Wills | 2008
Presentations
- The role of a case conceptualization model and core tasks of intervention | Donald Miechenbaum | 2014
- Transdiagnostic treatments for anxiety disorders | Martin Anthony | 2013
- The unified protocol for the transdiagnostic treatment of emotional disorders | Ellen Frank, Fiona Ritchey | 2015
- Making CBT Work (Working with your CBT therapist / Making your CBT therapist work with you) | Paul Salkovskis
Treatment Guide
- A manual of cognitive behavior therapy for people with learning disabilities and common mental disorders | Hassiotis, Serfaty, Azam, Martin, Strydom, King | 2012
Video
- CBT case formulation | Jacqueline Persons
Worksheets
- Cognitive Interpersonal Cycle Worksheet | Stirling Moorey | 2007
Recommended Reading
- Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognitive therapy and research, 36(5), 427-440
- Schema change processes in cognitive therapy | Padesky | 1994
- Wright, B., Williams, C., & Garland, A. (2002). Using the Five Areas cognitive–behavioural therapy model with psychiatric patients. Advances in Psychiatric Treatment, 8(4), 307-315.
- Williams, C., & Garland, A. (2002). Identifying and challenging unhelpful thinking. Advances in Psychiatric Treatment, 8(5), 377-386.
- Garland, A., Fox, R., & Williams, C. (2002). Overcoming reduced activity and avoidance: a Five Areas approach. Advances in Psychiatric Treatment, 8(6), 453-462.
- Williams, C., & Garland, A. (2002). A cognitive–behavioural therapy assessment model for use in everyday clinical practice. Advances in Psychiatric Treatment, 8(3), 172-179.
- A provider’s guide to brief cognitive behavioral therapy | Cully, Dawson, Hamer, Tharp | 2021
- Padesky, C. A., Mooney, K. A. (1990). Clinical tip: presenting the cognitive model to clients. International Cognitive Therapy Newsletter, 6, 13-14
- Arch, J. J., & Craske, M. G. (2009). First-line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatric Clinics of North America, 32(3), 525-547
What Is Cognitive Behavioral Therapy?
Assumptions of CBT
- people actively process information;
- our appraisals (the way that we think and interpret events) determine how we feel;
- dysfunctional thinking and biases in information processing (cognition/thinking) are responsible for the problems that people experience;
- different problems are associated with different cognitive themes (cognitive specificity theory): depression is associated with loss and defeat; anxiety is associated with danger and threat; obsessive-compulsive disorder is associated with inflated responsibility; substance abuse is associated with permissive beliefs; eating disorders are associated with self-criticism; social anxiety is associated with fear of evaluation; and PTSD is associated with appraisals of immediate threat;
- the thoughts that we have can be ‘distorted’ or biased. Common biases include over-generalization, arbitrary inference, selective abstraction, and catastrophizing;
- changing how we think and act will impact how we feel: cognition, emotion, and behavior interact in a reciprocal manner;
- psychopathology is a result of an interaction between stress and vulnerability;
- cognition happens at multiple levels (Alford & Beck, 1997) and all can influence the way that we feel and behave: preconscious, unintentional, automatic (e.g., negative automatic thoughts); the conscious level (e.g., if a patient is asked to explain the meaning of an automatic thought); and the metacognitive level (beliefs about beliefs);
- experiences, memories, thoughts, attitudes, and beliefs are encapsulated as ‘schemas’ and which may become activated and influence our perceptions and behaviors.
Principles of CBT
Judith Beck (1995) identified 11 principles of the practice of cognitive behavioral therapy, and these were expanded by Wills (2009):
- cognitive behavioral therapists use formulation to focus their therapeutic work
- cognitive behavioral therapists use formulation to tackle interpersonal and alliance issues
- cognitive behavioral therapy requires a sound therapeutic relationship
- cognitive behavioral therapists stress the importance of collaboration in the therapeutic relationship
- cognitive behavioral therapy is brief and time-limited
- cognitive behavioral therapy is structured and directional
- cognitive behavioral therapy is problem- and goal-oriented
- cognitive behavioral therapy initially emphasizes a focus on the present
- cognitive behavioral therapy uses an educational model
- homework and self-practice is a central feature of cognitive behavioral therapy (incorporating the use of CBT worksheets)
- cognitive behavioral therapists teach clients to evaluate and modify their thoughts
- cognitive behavioral therapy uses various methods to change cognitive content including thought records, behavioral experiments, surveys
- cognitive behavior therapy uses a variety of methods to promote behavioral change including exposure, behavioral experiments, role-play.
Procedures and Techniques of CBT
- Data gathering and symptom monitoring are used to understand problems and to measure change. CBT is an evidence-based approach that relies upon accurate data gathering regarding symptoms and experiences.
- Behavioral activation is a set of techniques for encouraging engagement in meaningful activity and is an effective treatment for depression.
- Case formulation is a method for understanding the origin and maintenance of a problem in cognitive and behavioral terms. CBT therapists may use a mixture of cross-sectional formulation to understand difficulties in the here-and-now, longitudinal formulation to understand the origins and precipitants of a problem, and cognitive behavioral models to understand the mechanisms underlying a problem.
- Cognitive restructuring describes techniques for changing what we think. It often involves the use of thought records, behavioral experiments, data gathering, or psychoeducation.
- Exposure is a technique from behavior therapy that is extensively used by CBT therapists, particularly for the treatment of anxiety. ‘Facing your fears’ is an essential behavioral component of CBT.
- Problem solving describes a series of techniques that are often taught as part of a CBT intervention. Effective problem solving helps people to make adaptive choices.
- Socratic methods are used by CBT therapists to help their clients explore what they know, and to form their own opinions on a topic. Aaron Beck encouraged the use of Socratic-like technique in his original treatment manual “use questioning rather than disputation and indoctrination … it is important to try to elicit from the patient what he is thinking rather than telling the patient what the therapist believes he is thinking” (Beck et al, 1979).
References
- Alford, B. A., & Beck, A. T. (1997). The relation of psychotherapy integration to the established systems of psychotherapy. Journal of psychotherapy integration, 7(4), 275-289.
- Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. New York: Guilford.
- Beck, J. S. (1995). Cognitive therapy: Basics and beyond. New York: Guilford.
- Wills, F. (2009). Beck’s cognitive therapy. CBT Distinctive Features Series. New York: Routledge.