Profile: Professor Christine Purdon Talks Compulsions And OCD

Professor Christine Purdon is a clinical psychologist, researcher and author with expertise in OCD, anxiety and CBT. She is the Director of Clinical Training for the University of Waterloo’s PhD program in Clinical Psychology, in Canada. We sat down with Christine to talk about the self-perpetuating cycle of compulsions. We discussed the importance of understanding compulsion goals, treatment implications, and leaving OCD in the waiting room.
Moments in time
Can you share some of the key moments that lead you to study compulsions?
When I started graduate school in 1990, I joined the lab of David A. Clark. Dr Clark worked directly with psychiatrist Aaron T. Beck, who is widely considered to be the founding father of cognitive behavior therapy (CBT). The CBT approach to understanding and treating mental health difficulties had not been widely adopted in 1990, and when I applied to graduate school there were only a handful of CBT therapists/researchers. I went to work with David at the University of New Brunswick, thinking I would study depression, but one day he said “There’s a really interesting area that I did my thesis on, it’s the study of ‘intrusive thoughts’, or, thoughts that resemble the obsessions experienced by people with OCD. There are only about 10 articles on intrusive thoughts, and I think it’s a really important area.” I began reading in this area immediately and realized how fascinating it was, and yet there were so few studies.I learned that the most people have obsessive thoughts, but only 1 to 2.5% of the population have OCD, and I started to wonder why intrusive thoughts affected people who are vulnerable to developing OCD differently. That caused me to shift from studying depression to studying intrusive thoughts.
At first, I concentrated on the appraisal of the obsession, because I thought that if you could detoxify the obsession, the compulsion would become obsolete. While understanding the appraisal of the obsession is important if you’re going to help the person, I soon realized that we paid almost no attention to compulsions.
By the early 90’s the cognitive model presented by Paul Salkovskis in 1985 had started to gain the momentum it deserved. His model helped us recognize that it’s not the content of the thought that causes OCD, but how people appraise their obsessions. OCD isn’t the result of somebody erroneously thinking that they’re going to hurt somebody. It’s their evaluation of the meaning and importance of having the thought that they might hurt someone that makes a difference. At this time, Paul Salkovskis and Jack Rachman were writing some elegant and wonderful papers. In fact, I would say that Salkovskis’ 1985 and 1989 papers on the theory of OCD are still the best papers available in terms of explaining the internal logic of OCD. As the cognitive model gained traction, people began researching appraisal of obsessions, but because this cognitive model of OCD was relatively new, we didn’t have a standard means of assessing appraisal. We were all trying to come up with our own different measures to identify and assess the appraisals that seemed to really drive OCD. During the World Congress of Behavioral and Cognitive Therapies/WCBCT conference in Copenhagen in 1995, Dave Clark and Mark Freeston suggested we form a working group to pool our efforts and develop a common measure of appraisal, and so the Obsessive Compulsive Cognitions Working Group was formed. At the first meeting, hosted at Smith College by Randy Frost and Gail Steketee, we identified the different areas of appraisal that we collectively thought were the most important. We then broke into working groups to identify the constructs within each area of appraisal, and ended up producing the Interpretation of Intrusions Inventory and the Obsessive Beliefs Questionnaire, which continue to be in use today.
At first, I concentrated on the appraisal of the obsession, because I thought that if you could detoxify the obsession, the compulsion would become obsolete. Although understanding the appraisal of the obsession is important if you’re going to help a person with OCD, I soon realized that we paid almost no attention to compulsions. I was unable to find research on even the basic phenomenology of compulsions, apart from one excellent book on the anatomy of obsessions and compulsions co-written by Jack Rachman. I thus had another opportunity to start looking into an area where there was barely any research. The most effective treatment for OCD is exposure and response prevention, but it’s only about 50% effective when you take treatment refusal and dropout into account. We had assumed that when a person comes to your door, they are ready to change and to tackle their OCD, and the first thing we told them is they can’t do their compulsions anymore, so it didn’t feel like we were serving people well. Meanwhile, despite all of our research on appraisal of obsessions had not improved our capacity to treat OCD did not change! The work wasn’t wasted, it had helped us to understand, conceptualize and formulate, but I felt there was something missing. We hadn’t accounted for how hard it was for people not to do their compulsions, and it became clear that there was a lot more going on with compulsions.

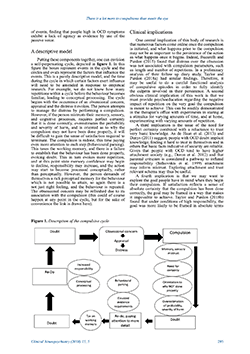
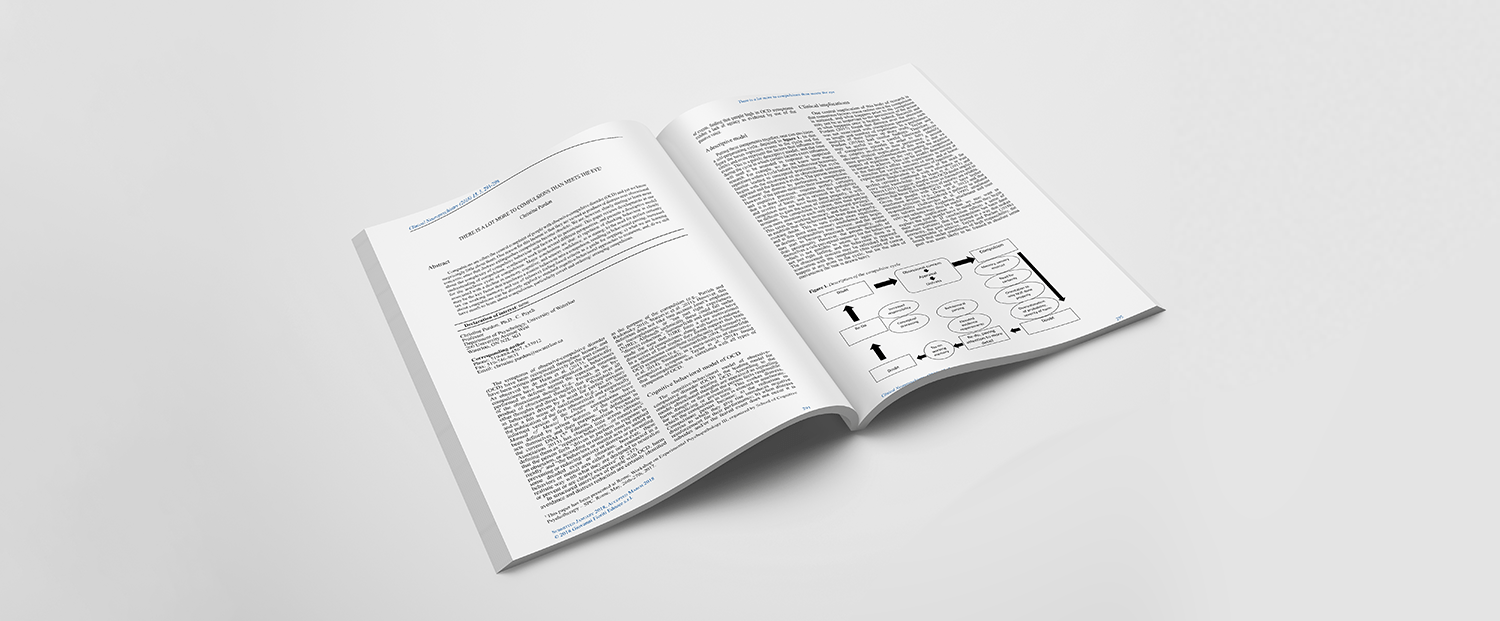
The model of the cycle of compulsion
What are the main elements in your cycle of compulsion?
The first element in the cycle concerns memory. People with OCD do not have poorer memory, but they do have poorer confidence in their memory of having carried out their compulsions. We know from the work of Adam Radomsky and Marcel van den Hout that repetition of checking behavior is associated with a decline in memory and confidence. This leads to more repetitions, but repeating an action erodes the confidence that it was carried out which in turn can foster greater repetition. Greater repetition results in familiarity which inhibits processing of the very details used to establish confidence in the memory. This is a basic cognitive process: when we do something repeatedly, we start to process it at a conceptual level, rather than the perceptual, and we know from memory and other cognitive research that over time conceptual processing suppresses perceptual processing.
The second key element is around the goal of the compulsion. People with OCD seek perfect, or near-perfect, certainty that a task been done properly. As they complete the task, they’re oriented to what might not have been right about it, plus they also have very high standards for getting it right, so they often feel the need to repeat it. It’s also been proposed that the more invested people are in achieving perfect certainty, the more evidence they require to make the decision to stop (also known as elevated evidence requirements). They ultimately end up taxing their working memory.
You can see how these key components together can create a self-perpetuating cycle of behavior. If someone can’t get the right feeling of confidence from doing their compulsion, they repeat it more. They then get lost and confused about whether they remember doing something the last time, or a different time, and because they keep repeating the same action, they’re starting to process it conceptually rather than perceptually, and losing the detail that they demand of themselves. In order to achieve that sense of confidence, they start to parse the behavior into very small actions. For most of us, washing our hands is one action (or, as I used to joke with my kids before CoVID, zero actions!) but for someone washing their hands compulsively, a hand wash could actually be 14 separate actions, each of which need to be done and remembered precisely. That’s a huge tax on working memory, so people lose track of whether they did everything, and have to keep repeating the behavior. This repetition can lead to a degeneration of confidence, and because their memory can’t produce what they’re asking of it, they start believing that they can’t trust their memory.
People with OCD are often trying to prevent harm in the future, but it’s impossible for them to establish that they have prevented that harm, so there’s no natural end for the behavior. They instead rely on a ‘felt sense’ of certainty.
Stanley J. Rachman pointed out in his 2002 paper that people with OCD are often trying to prevent harm in the future, but it’s impossible for them to establish that they have prevented that harm, so there’s no natural end for the behavior. They instead rely on a ‘felt sense’ of certainty. Examples of the most common termination criteria we hear are ‘I wash until it feels right / I wash until I feel satisfied / I wash until I’m certain’, but these are elusive feelings, which can’t be conjured intentionally, so they repeat the behavior until they get that right feeling. The more you repeat an action to solve a problem, the more you start to take ownership, and feel like it’s your problem to solve. If you repeat an action meant to prevent harm, you feel responsible we feel for preventing that harm, so now you have to make sure nobody gets cancer, etc. The obsession may then be refreshed at any point due to its association with the compulsion. That’s a very brief outline of the model for the cycle of the self-perpetuating mechanisms in OCD.
What implications did this cycle of compulsions have for you?
It got me thinking more! I realized our focus on the appraisal of obsessions meant we didn’t focus on the appraisal of what it means not to do the compulsion, or to stop it before you get that great sense of confidence. Working on obsession appraisals exclusively wasn’t working for my clients. They would do the easy part of exposure and would progress to some extent, but couldn’t go beyond a certain point, which meant that their OCD system was still intact. I also started to think more about people’s compulsion goals, and whether anybody had asked people with OCD what they are trying to accomplish when they did their compulsion? Were they trying to achieve a desired state (such as having clean hands) or were they trying to avoid an undesired state? Were they trying to reach certainty or to get rid of uncertainty? I think semantics and linguistics are really important here in terms of understanding how people frame their goal and what they’re trying to accomplish.
We did a lab study with people who had high fears of contamination, where we had a brand-new damp sponge, sitting in a little Tupperware container. We explained that the sponge may have come in contact with germs or bacteria, and asked the group to wipe their hands with the sponge before washing their hands. They had already been assigned to either shred paper or prepare little treat bags for the preschoolers in our building afterwards, but were asked to wash their hands first. We studied the washing behavior and during the hand wash we asked each person what their goal was. There were a some really interesting findings. Almost no one said they were trying to reduce distress or prevent harm, which is what the DSM states as the reason a compulsion is carried out. Their goals were very proximal: to ‘get their hands clean’, or ‘get rid of dirt and germs’. For people who had to prepare the treat bags afterwards, the goal was more likely to be framed in a way that made it impossible or unverifiable to achieve, saying their goals were to ‘ensure I get rid of all the germs’ or ‘make certain my hands are pure’, whereas people who were just going to be shredding paper had the same goal as anybody else, without OCD. That was really interesting, because we know people with OCD can and do function normally outside their obsessive-compulsive cycle.
In a second study, we asked people to time how long it took to carry out their compulsion and then answer a series of questions. We found that distress over the obsession had zero relationship to the amount of time they spent doing the compulsion, or the number of repetitions. This showed that the appraisal causes immediate distress that precipitates the compulsion, but once the compulsion starts, the initial distress doesn’t seem to matter anymore, as something else is kicking in. We also asked people about their deeper goals – how important was it that they avoid harm, or avoid feeling guilty? How important was it that they avoid being held responsible by other people? We found that the immediate goal is very proximal, ‘to get my hands clean, make sure the lights are off, make sure I’ve turned the stove off, make sure the water tap is off, etc.’, but the goal of avoiding being held responsible by others was the most important goal (far more than avoiding harm) and it was correlated with the goal of doing the compulsion properly. The proximal goal still needs to be accomplished in order to achieve the larger goal of distress and harm reduction, but this told us that the compulsion is not just about getting your hands clean. It’s more deeply felt than that – it’s about avoiding punishment and rejection from people.
At the same time, one of my students was doing an interview study with people about obsessional doubt, and asked, ‘what would it mean about you as a person if your doubt was true?’ The responses were very large, general, negative core beliefs: ‘it would mean I’m a terrible person, it would mean I’m a dangerous person, it would mean I’m an untrustworthy person, it would mean that you can’t rely on me.’ This shows that compulsion is a way of trying to establish that you’re a worthy person, hence the investment in getting the compulsion right. The initial cognitive appraisal model helps us understand why someone starts doing the compulsion, but this research helps us understand why people with OCD repeat the compulsion, why they are so driven and fraught. It’s because there’s this fear of being a terrible person, and this is one way they can control it and say, ‘I did this perfectly, so I’m an okay person today’.
What is most clinically useful about the compulsion cycle and your work on goals?
Firstly, the repetition effect helps people make sense of their own symptoms. Secondly, showing people why their goals are unverifiable or impossible can help them understand why they can’t be achieved, and how this leads them to rely on an internal felt sense that is very elusive. That’s all extremely useful in terms of helping them understand the persistence of the compulsion.
We should spend more time asking people about what it would mean if they didn’t do the compulsion, or if they stopped the compulsion before they got the right feeling.
In terms of treatment, it suggests we should spend more time asking people about what it would mean if they didn’t do the compulsion, or if they stopped the compulsion before they got the right feeling. For example, exposure-based models of treatment are based on trying to extinguish the distress over the obsession – your goal is to have the person be exposed to the obsession without doing the compulsion. If the distress declines over time, the compulsion is obsolete. This model suggests we should shift our focus with exposure to having the person do their compulsion once in a normal way, and stop before they get the desired internal felt sense.
Clinically I would also suggest focusing a lot more on helping clients to recognize that their compulsion is ego syntonic. People usually come to therapy because their compulsion is interfering with important goals in their life, but it is often also forwarding other goals. For example, the compulsion might be an expression of being a caring, loving person, but because the compulsions they do in the service of being loving and caring prevent them from leaving the house on time, they may be late for work and end up like looking unconscientious. Essentially, it’s the way that the compulsion undermines important goals that brings them to treatment. It’s important for us to acknowledge that the compulsion is also forwarding goals that reflect who the clients are as people and what’s important to them. Just saying, “you can’t do that anymore” can be a really hard sell for people. Clinically, our aim is to help people live their lives in line with their goals, without the requirement for absolute certainty, so I say to clients ‘Let’s not martyr yourself to get this perfect certainty’.
Talking to the belligerent OCD and other common challenges
What assumptions or misconceptions come up when you are working with students, and how do you handle them?
The one I come across all the time is that people get stuck with the content of the obsession. I once started working with someone in the medical profession who had developed a severe obsessional contamination concern that she was going to transmit a particular disease to her family. Most of her previous treatment had been talking about the probability of disease transmission and how irrational that was. That’s not the problem. The problem in OCD is that someone erroneously thinks they’re going to cause harm, and they require perfect certainty that they won’t cause harm to feel morally able to get on with their lives. As a result, they start to develop compulsive rituals that they have to do perfectly in order to feel like they’ve done everything they can. Once they start doing these rituals, self-perpetuating mechanisms kick in and prolong and cause this ritual to repeat. We shouldn’t be addressing the content of the OCD, but rather looking at the scaffolding that supports the OCD system. We worked on her ideas about the necessity and importance of feeling certain, and what it meant about her as a person if she didn’t have that certainty. We encouraged her to do her compulsion once, but then sit with the uncertainty and move along with her day without knowing for sure that her safety behavior of washing her hands before touching or hugging her children was sufficient or not, and she got much better.
Whenever I am working with somebody with OCD and I feel like we’re getting into arguments, it’s usually because I’m talking to the OCD, rather than the person … You can see when OCD is inhabiting the client by the change in their face: in their intensity, belligerence, and oppositional nature. If you keep engaging with the OCD and giving it airtime, it’ll take over the whole session. When you remind them that you don’t want to talk to their OCD, you can almost see their eyes clear.”
Whenever I am working with somebody with OCD and I feel like we’re getting into arguments, it’s usually because I’m talking to the OCD, rather than the person. I make that distinction from the beginning, ‘I want to talk to you. That means the person who recognizes they have a problem and doesn’t want to live their life in a prison anymore’. Once you’ve assessed the OCD you can hear what it has to say, but the OCD will want to ally with the client against you, whereas you want the client allied with you against the OCD. You can see when OCD is inhabiting the client by the change in their face: in their intensity, belligerence, and oppositional nature. If you keep engaging with the OCD and giving it airtime, it’ll take over the whole session. When you remind them that you don’t want to talk to their OCD, you can almost see their eyes clear. The assumption is that it’s the client that comes into the room and the OCD just sits in the waiting room, politely reading a magazine until the client comes back out again. It’s easy to forget that the OCD is in the room, and if it’s active, it’s going to be trying to direct the client. OCD is terrified of exposure and change.
It is essential that exposure be informed by the case formulation. Students can assume that just because a client is afraid of something, the client should be exposed to it. For example, if you have somebody who’s worried that they might be gay, they don’t want to look at gay pornography because they’re afraid of it, and so that gets put on the list for exposure. In fact, they don’t need to be comfortable with gay porn in order to get over their OCD, what they need exposure to is the uncertainty over whether or not they’re gay, without doing anything to try to resolve that uncertainty. You could use a magazine or something if you needed to evoke the obsessional concern, but your goal isn’t to get them to extinguish their fear to the magazine. Just because they’re afraid of it doesn’t mean it belongs on the hierarchy.
When doing contamination hierarchies, people often put things like eating a sandwich off a toilet seat on the list. I have a couple of perspectives on that. Others may disagree, but I don’t think people need to do things that are outside the norm in order to get better. Imagine having that at the top of a hierarchy: by session five the client knows that in two sessions they have to eat a sandwich off a toilet seat, and they’re already working out how to leave and never come back. Instead, focus on the factors that can vary the intensity of the need to do the component. If we ask them to shred paper in their study, they’re not at all worried about the cleanliness of their hands, but if they are going to prepare food, or hug their children, they are. I prefer to build a hierarchy around not doing the compulsion before certain actions. For example, they can start with not doing their compulsion giving their children a quick hug, then not doing it before giving them a longer hug, or not doing it before preparing food, and so on.
Teaching students to work on the case formulation is really important, as it helps arm the client with their own formulation so that they can make their own decisions. One of my supervisees had a client who was very worried about something happening to her in the shower and so she would leave the shower curtain wide open. This was a huge one for her to overcome. There had been discussion of a hierarchy of showering with the curtain eventually going from open to closed, but because she understood the model, she understood that the idea was to challenge what the OCD was saying to her about the meaning and importance of the shower curtain. Within one week, she was able to take three showers with the curtain completely closed, when she had estimated it would take her weeks to get to that point. As long as you and the client understand the causes and maintenance factors of OCD, empowering the client to make their own decisions is really powerful.
The brilliance of CBT is in an excellent formulation that is explanatory without being simplistic. It helps the person understand why they feel so strongly about their compulsion. It’s because they are trying to avoid feeling bad about themselves, it’s not just about getting their hands clean, or because they are crazy. Once you’ve understood what keeps OCD going, the treatment itself becomes more straightforward. One way I frame this to clients is to say: ‘Your OCD is behaving as if it’s a friend protecting you, but let’s talk about all the lies that it is telling you. You are giving the OCD more authority than you give yourself, so let’s work out why your OCD carries so much weight for you. If we can figure that out, we can start putting you in the driver’s seat instead.’ I think that’s a nice way to introduce the formulation and the cognitive aspect of OCD encapsulated within it.
Standing on the shoulders of giants
Do you feel more drawn towards research or clinical practice?
When I started, I assumed I would go into private practice, but I found the research really rewarding. Now I am a very committed scientist practitioner. I feel like I stand on the shoulders of giants, if you look at Aaron Beck, Paul Salkovskis, Jack Rachman, and Mark Freeston. It’s fascinating to launch from and elaborate on their fundamental core ideas, but you also need to be informed by clinical practice. Everyone I mentioned cares (or cared) deeply about client experience, and they approach the task with humility. The best people in this field are hugely attentive to what people with OCD are saying, and generate research questions based on what people tell us about their own experience. We cannot assume that we know what’s important to them, or what we should be researching to take away their suffering, without asking clients directly. I don’t think I would want to do research if I didn’t do clinical work, because I wouldn’t be asking the right questions. There are times when having an academic job and a private practice has felt overwhelming, but then I remember where my thinking was at when I was tempted to potentially shut down my practice, and I never did. My thinking would have stopped, it would be stagnant. Working with students is so rewarding – from sharing in their passionate enthusiasm, to seeing them grow and experience the joys of discovery, or even develop mastery.
What interests you at the moment?
One of the larger problems in OCD is that people don’t trust their own judgement. This ties back to something that we’re starting to understand more about, which is that there do seem to be links between attachment issues and OCD. There’s some really good research coming from Guy Doron, Mike Kyrios and others, looking at attachment and finding that people with OCD uniquely, and more so than people with other anxiety disorders, have anxious attachment. They also are more likely to report having had critical parents. You can see where the seeds of OCD can begin, when you have a child who shows their parent a drawing they’re really proud of and the parent criticizes it. Over time, they learn (A) they can’t tell what a good drawing is, or can’t trust their own judgement because Mom’s judgement is the best, and (B) if they don’t get that judgement right, they’re going to be criticized or punished. They learn that they need to find out what the external rules are in order to navigate their environment predictably and avoid punishment or feeling bad about themselves. They learn to find external rules to manage their own internal states.
What do you wish you had known when you were training, that you know now?
I used to be so worried about making sure everything I did in my sessions was always evidence-based, that I would often ignore my own instincts and instead go with what the manual said. There was one client in particular who (quite rightly) left treatment early, as I was unwilling to provide her with something because the manual said no. My instinct was to go with my case formulation idea, but instead I did what the manual said. I have a lot more confidence to go with my formulation now. We know the client. The manuals are general, they are there to help people with no background or training in CBT or the disorder to be able to use techniques we know work. Towards the beginning of your training it’s certainly worth keeping the manual in mind, but develop your own formulation, and don’t be afraid to use your own judgement based on that formulation, as long as your supervisors approve this for you. It takes time to be able to rely on your own your own feelings rather than the manual, but trusting in your own instincts and knowledge is an important rite of passage.