Safety Plan
Download or send
Tags
Languages this resource is available in
Problems this resource might be used to address
Techniques associated with this resource
Mechanisms associated with this resource
Introduction & Theoretical Background
Safety plans as a brief clinical intervention have a long history amongst people working with victims of domestic violence (e.g. Glander et al, 1998) and child abuse (e.g. Lipovsky et al, 1998). Amongst mental health professionals working with suicidal patients, safety plans are considered an important component of a comprehensive treatment plan: the intent of a safety plan is to help patients to lower their imminent risk of suicidal behavior. Henriques, Beck & Brown (2007) describe a safety plan as:
“a hierarchically arranged written list of coping strategies, developed collaboratively by the patient and therapist, which the patient can do if a crisis situation arises. At a minimum, the safety plan should include the telephone numbers of (a) social supports, (b) the therapist, (c) the on call therapist, (d) a local 24-hour emergency psychiatric center, and (e) other local support services that handle emergency calls. It should clearly communicate to
Therapist Guidance
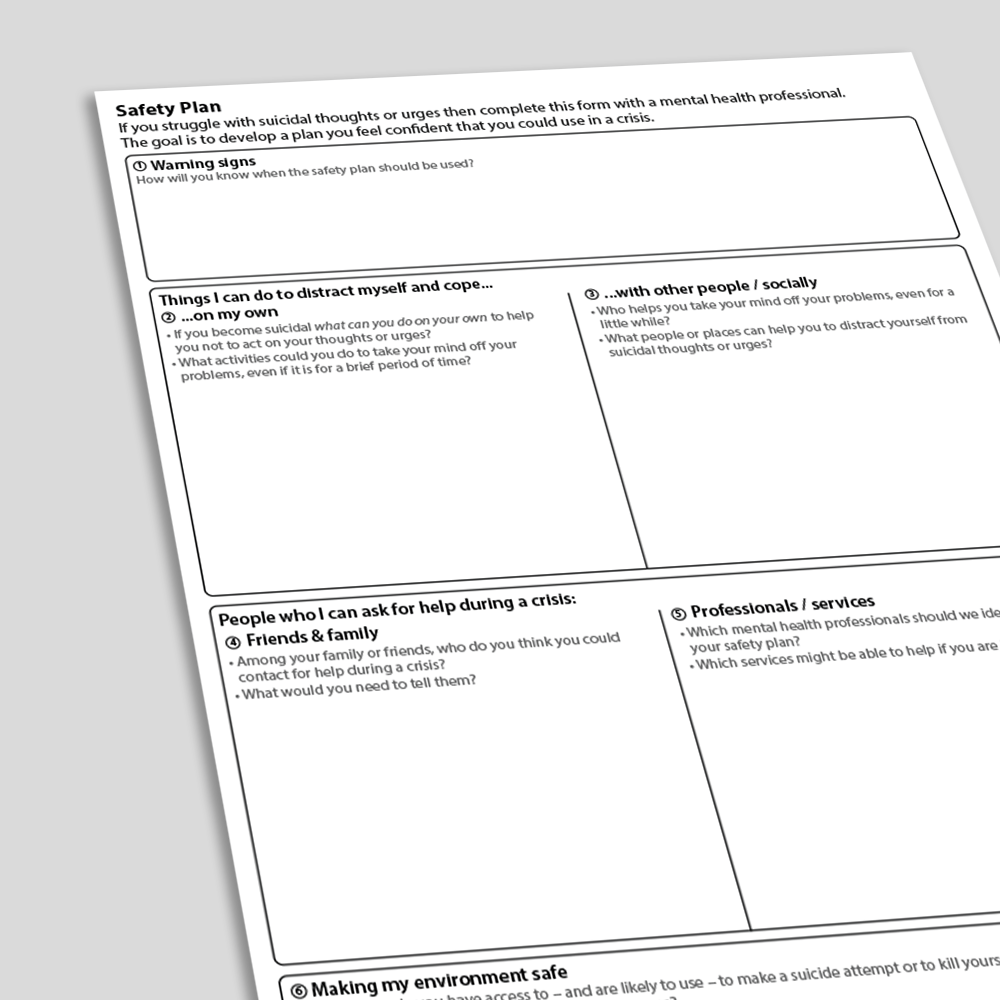
The Safety Plan exercise is best completed with patients following a comprehensive suicide risk assessment. It is most effective for clinicians to adopt a collaborative stance when completing a safety plan. The Safety Plan exercise can be completed in-session, and the clinician can use the attached prompt sheet to help them in guiding the patient through components of (i) recognizing triggers and warning signs, (ii) using internal coping strategies, (iii) using social contacts as distraction, (iv) contacting friends and family for help during a crisis, (v) contacting professionals to resolve a crisis, (vi) reducing access to lethal means, (vii) checking the likelihood that the patient will be able to implement the safety plan.
References And Further Reading
- Glander, S., Moore, M., Michielutte, R., & Parsons, L. (1998). The prevalence of domestic violence among women seeking abortion. Obstetrics & Gynecology, 91(6), 1002-1006.
- Henriques, G., Beck, A. T., & Brown, G. K. (2003). Cognitive therapy for adolescent and young adult suicide attempters. American behavioral scientist, 46(9), 1258-1268.
- Lipovsky, J. A., Swenson, C. C., Ralston, M. E., & Saunders, B. E. (1998). The abuse clarification process in the treatment of intrafamilial child abuse. Child Abuse & Neglect, 22(7), 729-741.
- Rudd, M. D., Mandrusiak, M., & Joiner Jr, T. E. (2006). The case against no‐suicide contracts: The commitment to treatment statement as a practice alternative. Journal of Clinical Psychology, 62(2), 243-251.
- Shaffer, D., & Pfeffer, C. R. (2001). Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. Journal of the American Academy of Child & Adolescent Psychiatry, 40(7), 24S-51S.
- Stanley, B., Brown, G. K., Karlin,